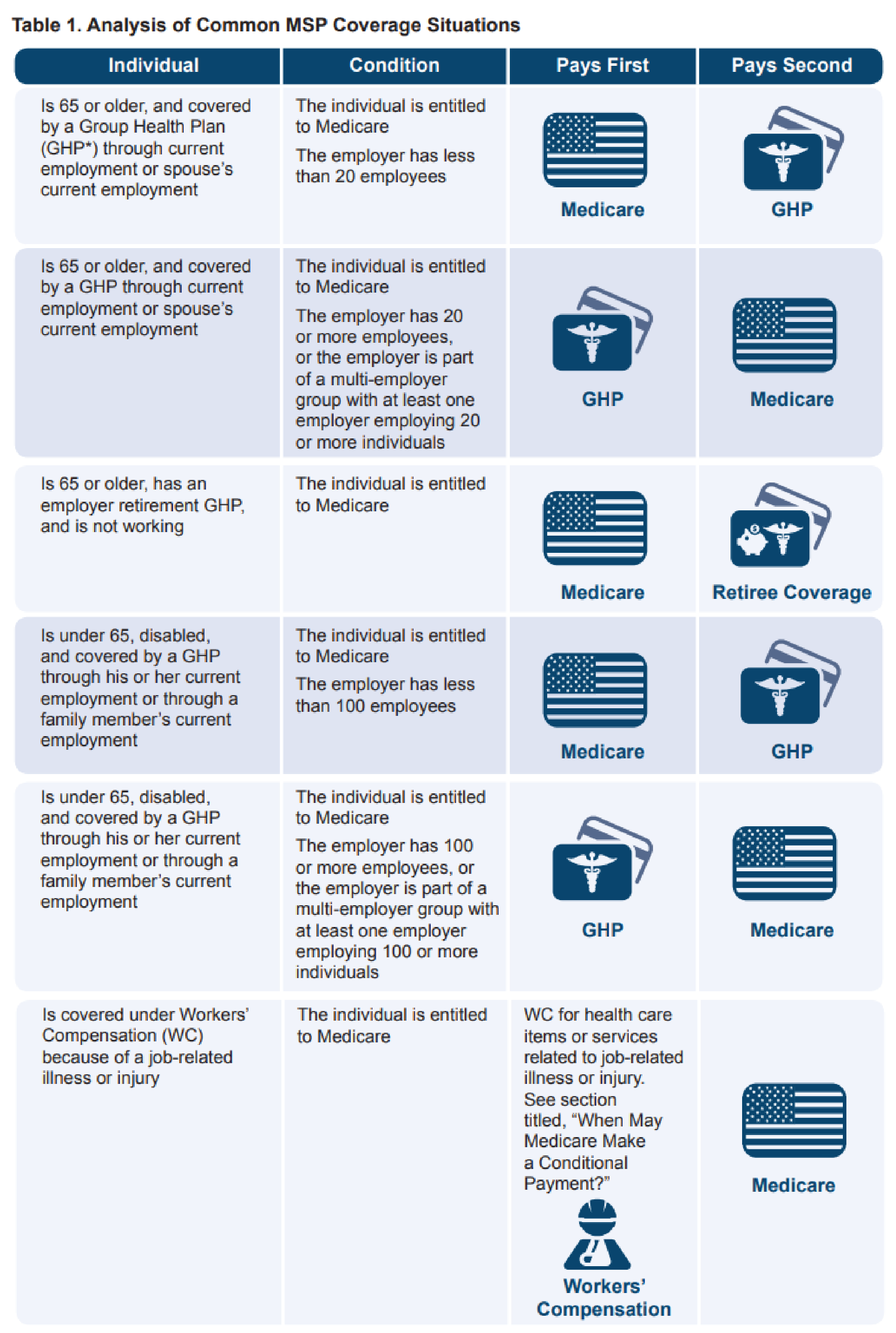
Medicare Secondary Payer Fact Sheet - What are a provider’s msp responsibilities? When must msp records be updated. The medicare secondary payer (msp) rules are complex and. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. How do i identify payers primary to medicare? Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. What is msp and what are the msp provisions?
What is msp and what are the msp provisions? Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. When must msp records be updated. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. How do i identify payers primary to medicare? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. The medicare secondary payer (msp) rules are complex and. What are a provider’s msp responsibilities? Any entity providing items and services to medicare patients must determine if medicare is the primary payer.
The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. How do i identify payers primary to medicare? What is msp and what are the msp provisions? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. What are a provider’s msp responsibilities? Any entity providing items and services to medicare patients must determine if medicare is the primary payer. The medicare secondary payer (msp) rules are complex and. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. When must msp records be updated. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
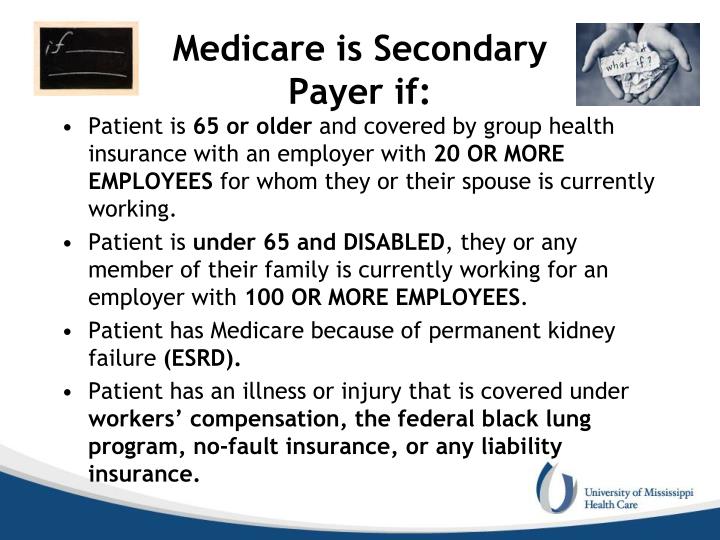
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. What are a provider’s msp responsibilities? How do i identify payers primary to medicare? The medicare secondary payer (msp) rules are complex.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
Any entity providing items and services to medicare patients must determine if medicare is the primary payer. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare..
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
What are a provider’s msp responsibilities? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and.
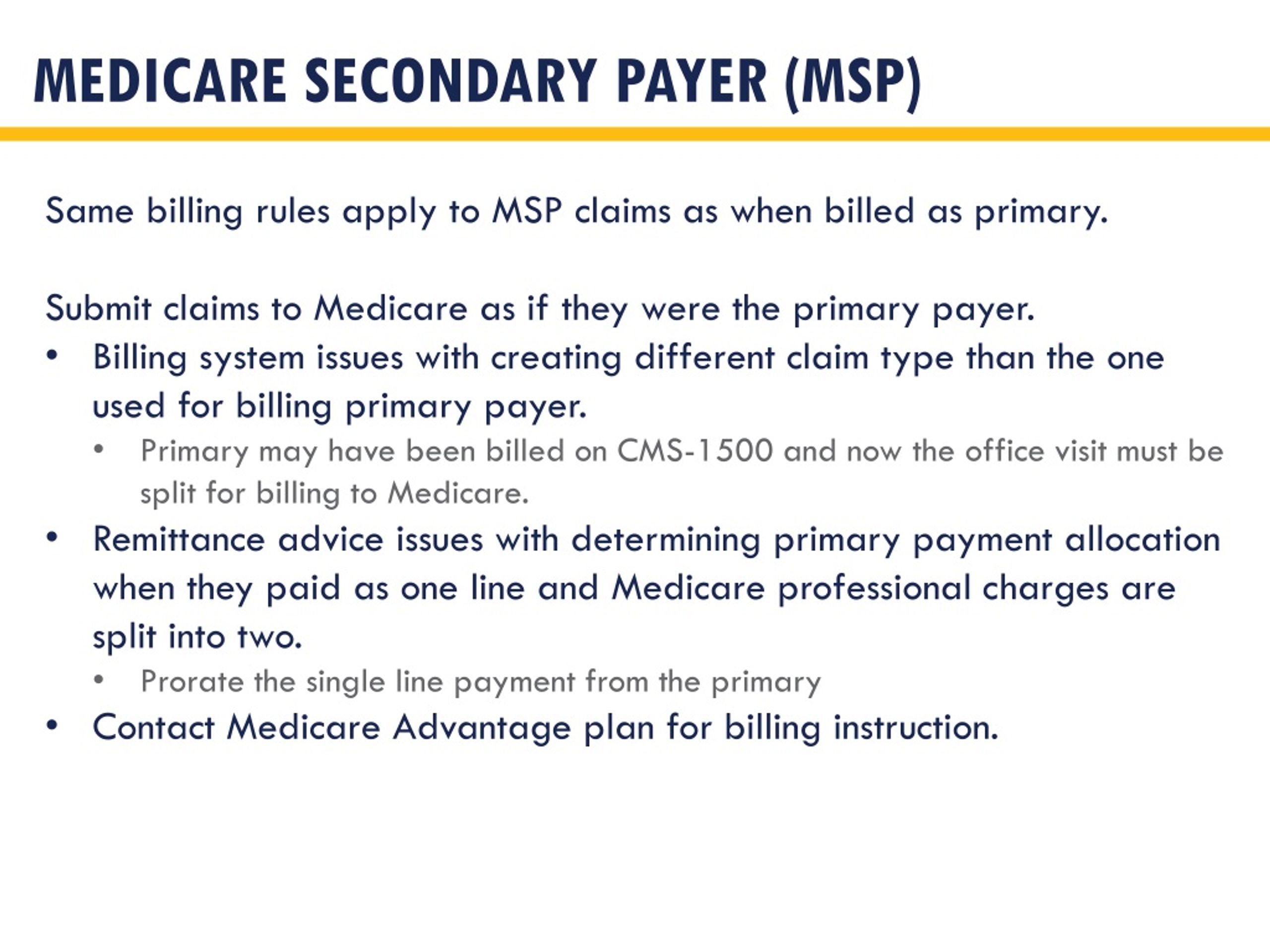
PPT RHC BILLING 101 PowerPoint Presentation, free download ID1595196
What is msp and what are the msp provisions? Any entity providing items and services to medicare patients must determine if medicare is the primary payer. What are a provider’s msp responsibilities? Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you.
PPT Provider based billing PowerPoint Presentation, free download
The medicare secondary payer (msp) rules are complex and. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals.
PPT CHAA Examination Preparation PowerPoint Presentation ID4372885
The medicare secondary payer (msp) rules are complex and. What is msp and what are the msp provisions? Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. Any entity providing items.
PPT Chapter 12 Commercial Insurance PowerPoint Presentation, free
When must msp records be updated. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. What is msp and what are the msp provisions? Any entity providing items and services to.
PPT MSP Presentation Background & Basics Presented by Keith Ewing
Any entity providing items and services to medicare patients must determine if medicare is the primary payer. The medicare secondary payer (msp) rules are complex and. How do i identify payers primary to medicare? What is msp and what are the msp provisions? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such.
What is Medicare Secondary Payer? Ametros
The medicare secondary payer (msp) rules are complex and. How do i identify payers primary to medicare? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. What is msp and what are the msp provisions? Pursuant to 42 cfr § 411.100,.
Understanding Medicare Secondary Payer (MSP)
What is msp and what are the msp provisions? Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. When must msp records be updated. What are a provider’s.
Medicare Secondary Payer (Msp) Provisions Protect Medicare From Paying When Another Entity Should Pay First.
How do i identify payers primary to medicare? When must msp records be updated. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance.
The Centers For Medicare & Medicaid (Cms) Has Rules For Determining When Other Types Of Insurance Such As An Employer’s Group Health Plan Must Pay Primary To Medicare.
What are a provider’s msp responsibilities? What is msp and what are the msp provisions? The medicare secondary payer (msp) rules are complex and. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or.